Neck Pain and Chiropractic
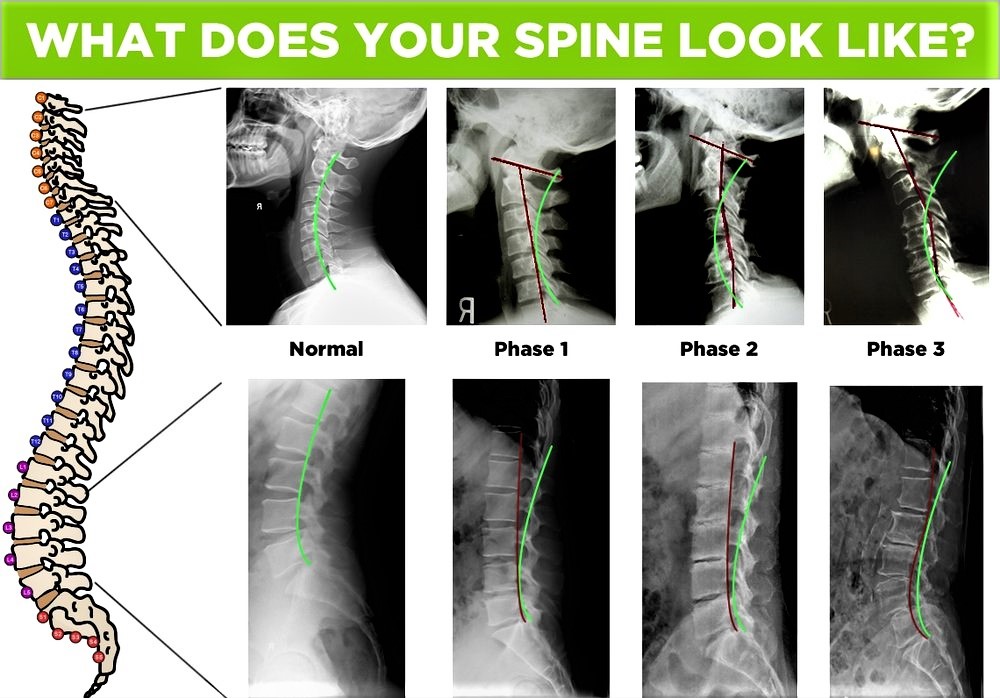
Our neck, also called the cervical spine, begins at the base of the skull and contains seven small vertebrae. Incredibly, the cervical spine supports the full weight of your head, which is on average about 12 pounds. While the cervical spine can move your head in nearly every direction, this flexibility makes the neck very susceptible to pain and injury.
The neck’s susceptibility to injury is due in part to biomechanics. Activities and events that affect cervical biomechanics include extended sitting, repetitive movement, accidents, falls and blows to the body or head, normal aging, and everyday wear and tear. Neck pain can be very bothersome, and it can have a variety of causes.

Here are some of the most typical causes of neck pain:
- Injury and Accidents: A sudden forced movement of the head or neck in any direction and the resulting “rebound” in the opposite direction is known as whiplash. The sudden “whipping” motion injures the surrounding and supporting tissues of the neck and head. Muscles react by tightening and contracting, creating muscle fatigue, which can result in pain and stiffness. Severe whiplash can also be associated with injury to the intervertebral joints, discs, ligaments, muscles, and nerve roots. Car accidents are the most common cause of whiplash.

- Growing Older: Degenerative disorders such as osteoarthritis, spinal stenosis, and degenerative disc disease directly affect the spine.
- Osteoarthritis, a common joint disorder, causes progressive deterioration of cartilage. The body reacts by forming bone spurs that affect joint motion.
- Spinal stenosis causes the small nerve passageways in the vertebrae to narrow, compressing and trapping nerve roots. Stenosis may cause neck, shoulder, and arm pain, as well as numbness, when these nerves are unable to function normally.
- Degenerative disc disease can cause reduction in the elasticity and height of intervertebral discs. Over time, a disc may bulge or herniation, causing tingling, numbness, and pain that runs into the arm.
Daily Life: Poor posture, obesity, and weak abdominal muscles often disrupt spinal balance, causing the neck to bend forward to compensate. Stress and emotional tension can cause muscles to tighten and contract, resulting in pain and stiffness. Postural stress can contribute to chronic neck pain with symptoms extending into the upper back and the arms.
Chiropractic Care of Neck Pain
During your visit, your doctor of chiropractic will perform exams to locate the source of your pain and will ask you questions about your current symptoms and remedies you may have already tried. For example:
- When did the pain start?
- What have you done for your neck pain?
- Does the pain radiate or travel to other parts of your body?
- Does anything reduce the pain or make it worse?
Your doctor of chiropractic will also do physical and neurological exams. In the physical exam, your doctor will observe your posture, range of motion, and physical condition, noting movement that causes pain. Your doctor will feel your spine, note its curvature and alignment, and feel for muscle spasm. A check of your shoulder area is also in order. During the neurological exam, your doctor will test your reflexes, muscle strength, other nerve changes, and pain spread.
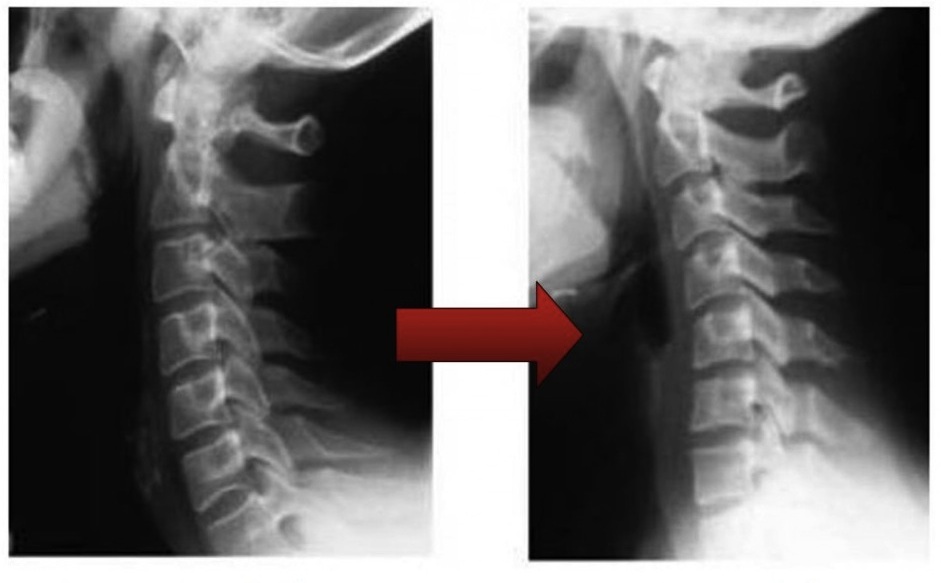
In some instances, your chiropractor might order tests to help diagnose your condition. An x-ray can show narrowed disc space, fractures, bone spurs, or arthritis. A computerized axial tomography scan (a CT or CAT scan) or a magnetic resonance imaging test (an MRI) can show bulging discs and herniations. If nerve damage is suspected, your doctor may order a special test called electromyography (an EMG) to measure how quickly your nerves respond.
Doctors of chiropractic are conservative care doctors; their scope of practice does not include the use of drugs or surgery. If your chiropractor diagnoses a condition outside of this conservative scope, such as a neck fracture or an indication of an organic disease, he or she will refer you to the appropriate medical physician or specialist. He or she may also ask for permission to inform your family physician of the care you are receiving to ensure that your chiropractic care and medical care are properly coordinated.
Neck Manipulation

A neck manipulation (also known as cervical adjustment) is a precise procedure applied to the joints of the neck, usually by hand. A neck adjustment works to improve the mobility of the spine and to restore range of motion; it can also increase movement of the adjoining muscles. Patients typically notice an improved ability to turn and tilt the head, and a reduction of pain, soreness, and stiffness.
Of course, your chiropractor will develop a program of care that may combine more than one type of treatment, depending on your personal needs. In addition to manipulation, the treatment plan may include mobilization, massage or rehabilitative exercises, or something else.
Back Pain Prevention & Treatment

Back pain is a fact of life for many people. Research shows that up to 80% of the population will experience back pain at some point during their lives.1 It is also the second most common reason for visits to the doctor’s office, outnumbered only by upper-respiratory infections.
Sometimes back pain is sharp and intense, caused by a wrong move or an injury, and heals in a few days or weeks. Others experience back pain as a chronic condition, seriously altering their ability to work and enjoy time with family, friends and other leisure activities—leading to depression in some cases. A recent global survey of health conditions identified back pain as the single most disabling condition worldwide.
Moreover, as lifestyles have become more sedentary and the rate of obesity has risen, back pain has become increasingly prevalent, even among young children.
Spinal health is an important factor in preventing back pain, as well as maintaining overall health and well-being.
Things such as better nutrition, exercise, ergonomic workspaces and proper lifting and movement techniques can go a long way in helping people to strengthen their spines and potentially avoid serious injury and chronic pain. When back pain hits, research shows that a conservative approach to treatment is the best option.
Conservative Treatment Options Supported by Research
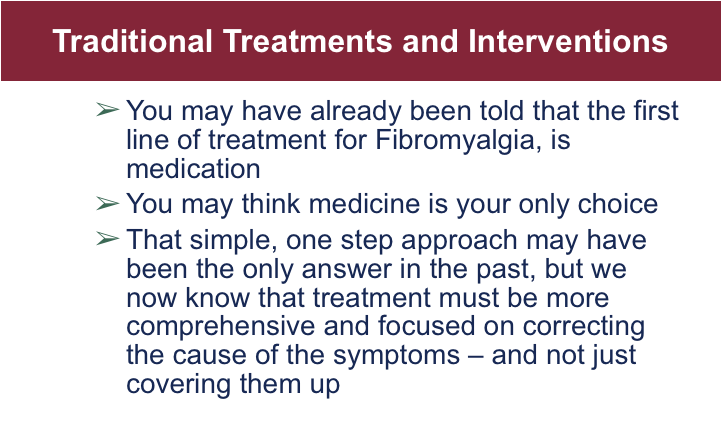
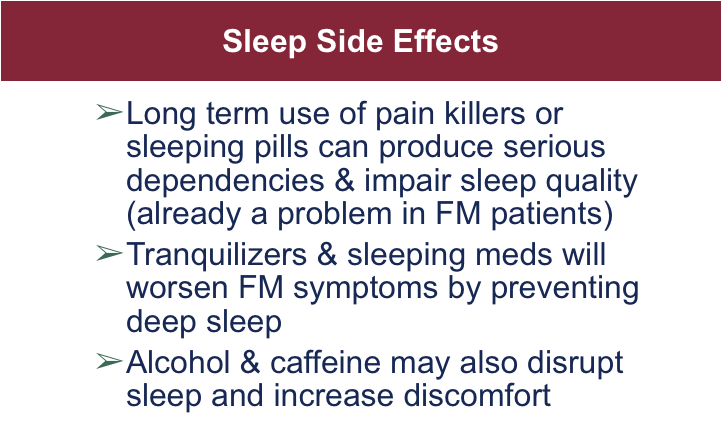
Treatment for back pain has come a long way. It was once believed that taking pain medication and getting some rest and relaxation were the best course of treatment for a bout of low-back pain, but nowadays research supports first trying drug-free, conservative options for pain management while remaining as active as possible during recuperation.
The epidemic of prescription opioid overuse and abuse has also led many health groups to reconsider the value of a conservative approach to common conditions such as back pain. For example, the American College of Physicians (ACP), the largest medical-specialty society in the world, updated its back pain treatment guidelines to support a conservative approach to care.
In March 2016, the Centers for Disease Control and Prevention released updated guidelines for prescribing opioids that also promote the use of non-pharmacologic alternatives for the treatment of chronic pain. In 2015, the Joint Commission, the organization that accredits more than 20,000 health care systems in the U.S. (including every major hospital), recognized the value of non-drug approaches to pain management by adding chiropractic and acupuncture to its pain management standard.
Beyond the risks of overuse and addiction, prescription drugs that numb pain may also convince a patient that a musculoskeletal condition such as back pain is less severe than it is, or that it has healed. That misunderstanding can lead to over-exertion and a delay in the healing process or even to permanent injury.
With the steep costs associated with prescription drugs, chiropractic’s conservative approach makes economic sense as well. A recent 2012 study found that spinal manipulation for neck and back pain was cost-effective used either alone or combined with other therapies first.
Another study based on Washington state workers found that 42.7 percent of people who visited a surgeon first for work-related back pain eventually had surgery, compared to only 1.5 percent of those who visited a chiropractor first.
Chiropractic is a health care profession that focuses on disorders of the musculoskeletal system and the nervous system, and the effects of these disorders on general health.

Chiropractic services are used most often to treat conditions such as back pain, neck pain, pain in the joints of the arms or legs, and headaches. Chiropractors practice a hands-on, drug-free approach to health care that includes patient examination, diagnosis and treatment.
Widely known for their expertise in spinal manipulation, chiropractors are also trained to recommend therapeutic and rehabilitative exercises, and to provide nutritional, dietary and lifestyle counseling.
History of Chiropractic Treatment for Back and Neck Pain in America

Since its inception in 1895, American Chiropractic has provided treatment for patients with back pain, neck pain and headache. Throughout American chiropractic history, some chiropractors have claimed a relationship among the spine, nervous system and brain as essential to one’s health and have held that structural imbalances within the spine can affect functioning with the spinal cord, nerves, muscles, bones and joints of the body.
Over the years, based on evidence from the scientific literature, chiropractic physicians have increasingly focused on evidence-based treatment of spine-related disorders as well as other musculoskeletal problems.
Chiropractic treatment has traditionally been based on spinal manipulation, which generally involves applying a manual, controlled force into joints that have become restricted by tissue injury with the purpose of restoring the joint’s mobility, alleviating related pain and tightness, and allowing the tissues to heal.
While spinal manipulation has become more specialized since its earliest applications in chiropractic care, it has remained one of the most commonly used chiropractic treatments of a profession that does not prescribe medication or perform surgery.
However, as chiropractic doctors have evolved with the emerging evidence as to the most effective approaches to back pain, neck pain and headaches, they have embraced a variety of evidence-based treatment approaches.
A number of chiropractors have obtained additional degrees such as PhD’s and have begun to investigate the effects of manipulation as well as other treatments provided by chiropractors.
Spinal Manipulation in American Chiropractic History
Spinal manipulation was not invented by a chiropractor, nor is it even a new or recent method. Manipulation of the spine dates back to the beginning of recorded time, with Hippocrates once noting it as a key to treating diseases.
Spinal manipulation is often associated with chiropractic care because of a man named Daniel David (D.D.) Palmer, the founder of chiropractic in the United States. Prior to the 20th century, Palmer maintained an interest in the spine’s role on health and began to study its anatomy, learn more about the use of spinal manipulation in ancient times, and teach himself how to manipulate the spine.
In 1895, Palmer was approached by a janitor who was deaf in one ear. Palmer theorized that the condition was likely related to the spine, possibly a displaced vertebra.
According to many historical accounts, Palmer examined the man’s back, noticed a bump near the spine, and manipulated the area. The hands-on adjustment was reported by Palmer to quickly restore the man’s hearing. This event is considered the start of chiropractic history.
A combination of the Greek words “cheir” (hand) and praktos (“done”), chiropractic means “Done by Hand”, although it is important to note that modern spinal manipulation has expanded beyond just hands-based adjustments.
In 1907, Palmer added the term “subluxation” to the chiropractic vocabulary. Palmer explained “subluxations” in terms of the spinal vertebrae and joints putting pressure on the nerves, thus impairing functioning, and then detailed how spinal adjustments could be used to reduce subluxation and improve patient symptoms.
Subluxation is still used today by some chiropractors to describe specific misalignments of the spinal vertebrae and joints and to determine appropriate treatment options. Other terminology currently in use includes manipulative lesion, spinal dysfunction, or joint dysfunction.
At least one chiropractic school (National University of Health Sciences) has begun to refer to the term “subluxation” from a historical perspective only.
American Chiropractic History in the 20th and 21st Century
In 1897, Palmer founded the Palmer School of Chiropractic (which still exists today) to teach students about chiropractic principles and train them in chiropractic manipulation.
Palmer’s son Bartlett Joshua (B.J.) further developed and promoted chiropractic in the first half of the 20th century. B.J. Palmer not only provided training in chiropractic, but aided in the education of both the medical community and the general public on the profession.
During this time, chiropractic gradually grew in popularity for patients seeking alternatives to traditional treatments using drugs, and its core principles slowly gained more acceptance with continued research.
By the late 20th century, chiropractic emerged as one of the most popular and accessible forms of health care.
Arthritis: Stop, Prevent, or Reverse It






















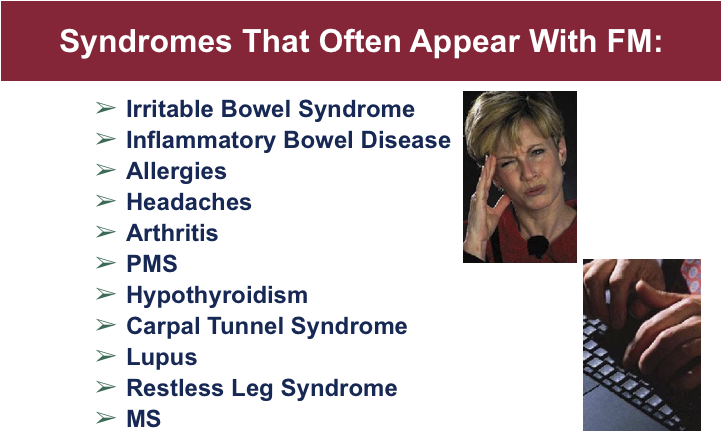
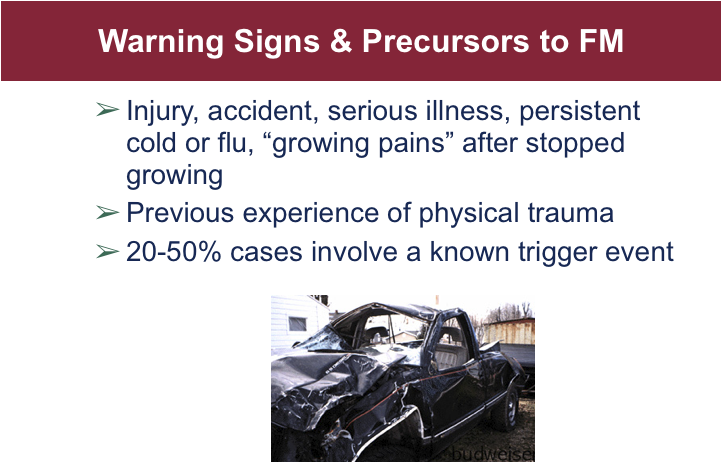
Eliminating the Pain of Fibromyalgia
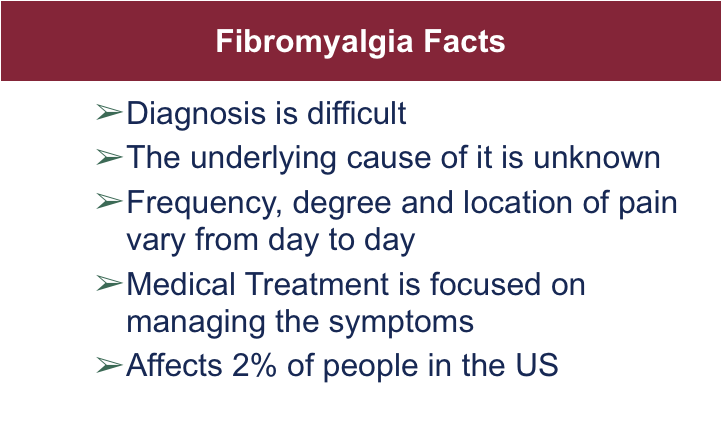
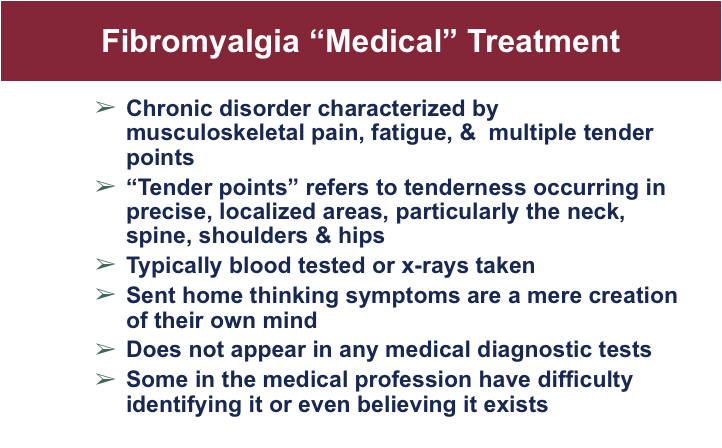
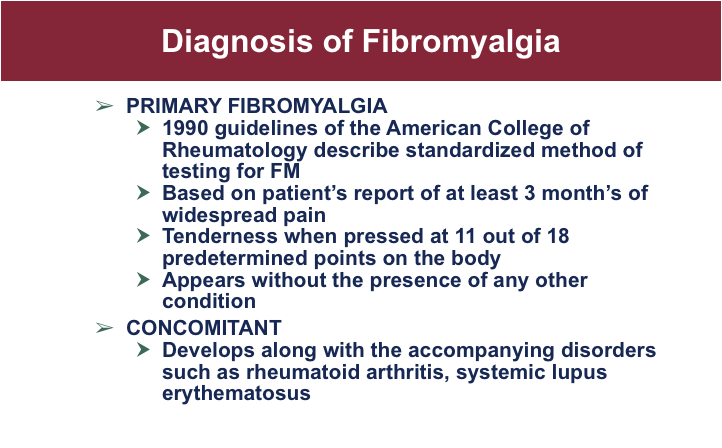
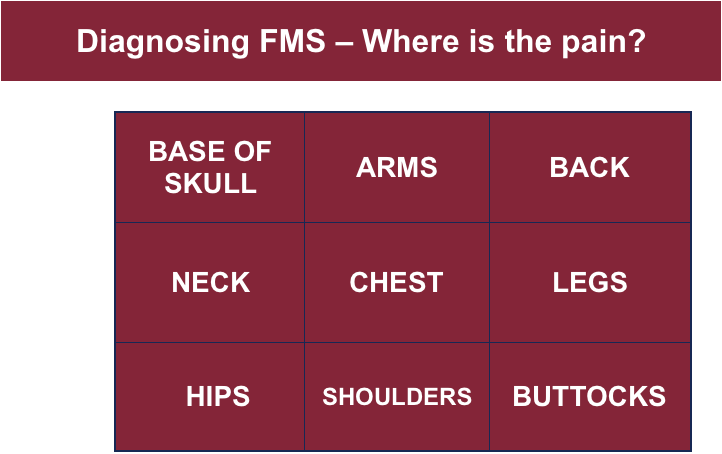
Diagnosing FMS – Where is the pain?
Myofascial Pain Syndrome as Fibromyalgia


Who are Doctor of Chiropractors?
Doctors of Chiropractic (DCs) – often referred to as chiropractors or chiropractic physicians – practice a hands-on, drug-free approach to health care that includes patient examination, diagnosis and treatment. Chiropractors have broad diagnostic skills and are also trained to recommend therapeutic and rehabilitative exercises, as well as to provide nutritional, dietary and lifestyle counseling.
DCs may assess patients through clinical examination, laboratory testing, diagnostic imaging and other diagnostic interventions to determine when chiropractic treatment is appropriate or when it is not appropriate. Chiropractors will readily refer patients to the appropriate health care provider when chiropractic care is not suitable for the patient’s condition, or the condition warrants co-management in conjunction with other health care providers.
In many cases, such as lower back pain, chiropractic care may be a patient’s primary method of treatment. When other medical conditions exist, chiropractic services may complement or support medical treatment by relieving the musculoskeletal aspects associated with the condition.
Like their MD colleagues, doctors of chiropractic are subject to the boundaries established in state practice acts and are regulated by state licensing boards. Further, their education in four-year doctoral graduate school programs is nationally accredited through an agency that operates under the auspices of the U.S. Department of Education. After graduation, they must pass national board exams before obtaining a license to practice, and then must maintain their license annually by earning continuing education (CE) credits through state-approved CE programs.
Chiropractic Qualifications
Educational and licensing requirements for doctors of chiropractic (DCs) are among the most stringent of any of the health care professions.
DCs are educated in nationally accredited, four-year doctoral graduate school programs through a curriculum that includes a minimum of 4,200 hours of classroom, laboratory and clinical internship, with the average DC program equivalent in classroom hours to allopathic (MD) and osteopathic (DO) medical schools.
Chiropractors are designated as physician-level providers in the vast majority of states and federal Medicare program. The essential services provided by DCs are also available in federal health delivery systems, including those administered by Medicaid, the U.S. Department of Veterans Affairs, the U.S. Department of Defense, the Federal Employees Health Benefits Program, Federal Workers’ Compensation, and all state workers’ compensation programs.
Chiropractic Education
The typical applicant at a chiropractic college has already acquired nearly four years of pre-medical undergraduate college education, including courses in biology, inorganic and organic chemistry, physics, psychology and related lab work. Once accepted into an accredited chiropractic college, the requirements become even more demanding — four to five academic years of professional study are the standard. Because of the hands-on nature of chiropractic, and the intricate adjusting techniques, a significant portion of time is spent in clinical training.
Chiropractors undergo a rigorous education in the healing sciences, similar to that of medical doctors. In some areas, such as anatomy, physiology, rehabilitation, nutrition and public health, they receive more intensive education than their MD counterparts. Like other primary health care doctors, chiropractic students spend a significant portion of their curriculum studying clinical subjects related to evaluating and caring for patients. Typically, as part of their professional training, they must complete a minimum of a one-year clinical-based program dealing with actual patient care. In total, the curriculum includes a minimum of 4,200 hours of classroom, laboratory and clinical experience. The course of study is approved by an accrediting agency, the Council on Chiropractic Education, that is recognized by the U.S. Department of Education.
This extensive education prepares doctors of chiropractic to diagnose health care conditions, treat those that are within their scope of practice and refer patients to other healthcare practitioners when appropriate.
Certification and Licensure
Certification is managed by the National Board of Chiropractic Examiners (NBCE), which administers national board exams that graduates of accredited chiropractic colleges must pass before applying for a state license to practice. Licensure is managed by individual states, which have varying requirements. Most states require chiropractors to meet yearly continuing education requirements to maintain their license.
Can Chiropractic Help You?



















Facts About Low Back Pain
Low Back Pain Incredible Non-Surgical, Drug-Free Solution

Facts About Low Back Pain

Facts About Low Back Pain



Virtually all human beings are subject to back problems.
The fact that humans walk upright, on two legs, puts great pressure on the spine and muscles that support it.
Chronic Back Pain can Affect Us…

Causes of Back Pain


Causes of Back Pain
Accidents
Auto
Lifting
Sports
Subluxation (discussed later)
Disease
Infection
Tumor
Bad “back habits” as unnecessary strain from overexertion at play or work:
Lifting, pushing, pulling, and reaching for things improperly,
Poor standing and sitting posture
Conditions Causing Back Pain
Pinched or Irritated Nerves
Bulging or Herniated Discs
Degenerated Discs
Scoliosis
Arthritis
Muscle Pain
Subluxation
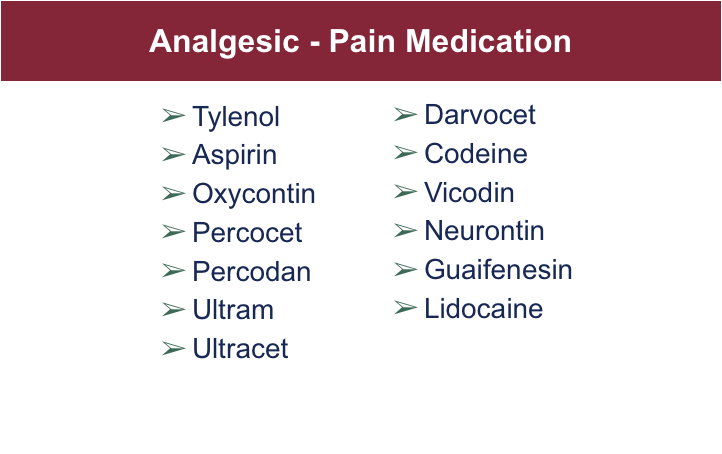
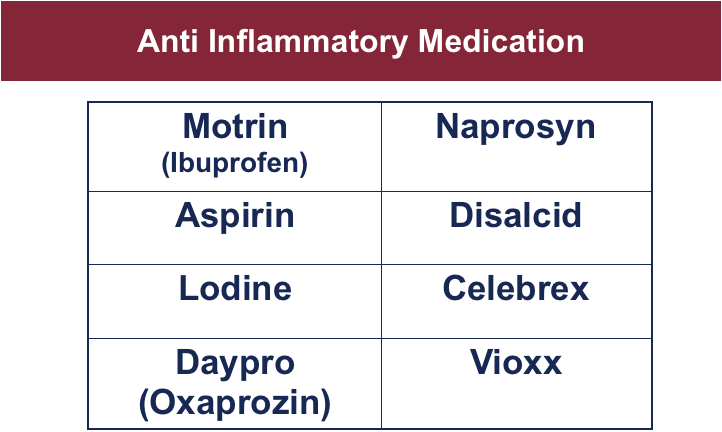
Treatment through Medication

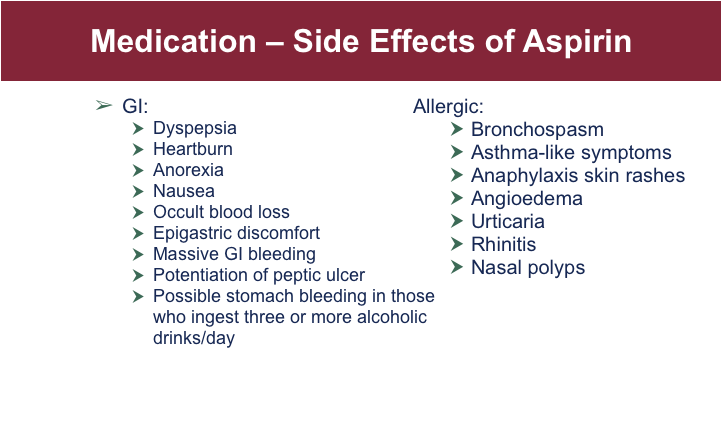
Aspirin Side-Effects
GI: Dyspepsia, heartburn, anorexia, nausea, occult blood loss, epigastric discomfort, massive GI bleeding, potentiation of peptic ulcer. Possible stomach bleeding in those who ingest three or more alcoholic drinks/day.
Allergic: Bronchospasm, asthma-like symptoms, anaphylaxis skin rashes, angioedema, urticaria, rhinitis, nasal polyps.
Hematologic: Prolongation of bleeding time, thrombocytopenia, leukopenia, purpura, shortened erythrocyte survival time, decreased plasma iron levels.
Miscellaneous: Thirst, fever, dimness of vision.
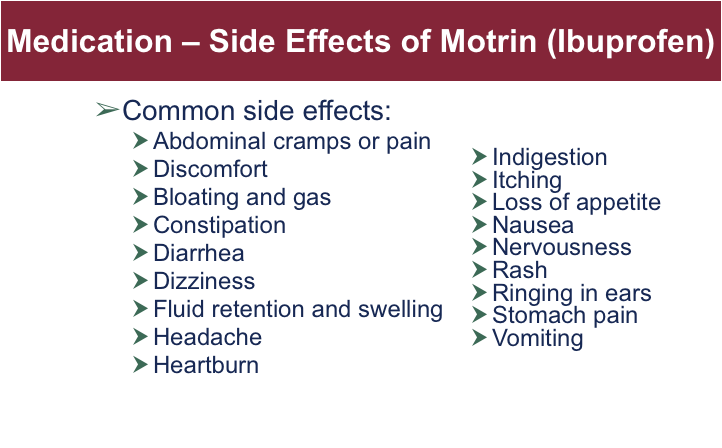
Motrin (Ibuprofen) Side-Effects
Treatment Through Medication
Most common effects include:
Abdominal cramps or pain,
Bloating and gas,
Constipation, diarrhea
Dizziness
Fluid retention and swelling,
Headache,
Heartburn, indigestion
Itching, Rash,
Loss of appetite,
Nausea, vomiting
Anxiety
Ringing in ears
There are also, more serious, but less common side effects

NSAIDs like Advil and Tylenol have shown to cause serious GI problems in 1,000 to 4,000 people per million
Reportedly 7,600 patients die annually from their use.
Other Treatments
Other treatments may give short term relief but none have been found to speed recovery or keep acute back problems from returning. They may also be expensive, they include:
Traction
TENS
Massage
Biofeedback
Acupuncture
Back injections
Back corsets
Ultrasound
Surgical Treatment

Can Chiropractic Help?
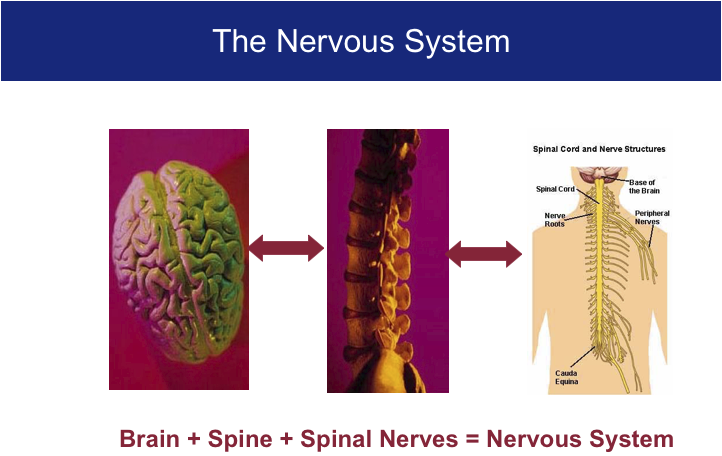
Understanding The Master Control System?
What coordinates every function within the body.
Nervous System
“Every function of the human body is under the control of the nervous system. Its function is to coordinate all the other organs and structures and to relate the individual to his environment.”
“The nervous system controls and coordinates all functions of the body.”
The MASTER System
Your BRAIN, SPINE, and SPINAL NERVES make up your body’s MASTER control system. When the nervous system is FREE of all interference, your body can function at its MAXIMUM level. When there is nerve interference in the spine, dis-ease or disharmony occurs
The Nervous System

Communications From Your Spine

Nervous System Imbalance

Nervous System Interference
Oftentimes, nervous system interference can occur as a result of birth trauma, stress, falls, deficiencies, outside pathogens, auto-intoxication, or immune dysfunction. These imbalances can manifest as mental or emotional disorders, discomfort, distress, and/or pain
Blown Circuits?
Your circuit breaker box in your house is just like your spine!
How? Just as each circuit controls a specific room in your house…each vertebrae (all 24) sends a “wire” that we call a nerve to each and every muscle organ, gland, and cell in your body
Your Spinal Circuitry
If a vertebrae should move out of place (subluxate), you will have nerve interference that can act like a blown circuit by interfering with the instructions, information, directions, and nerve impulses being sent by the brain – thereby causing the end-organ that is controlled by those nerves to dys-function
Vertebral Subluxations

3 Causes of Vertebral Subluxation

WE Know That…….

WE Also Know That…….
In order to have maximum Health and Function, you need to have:
Plenty of Sleep
Consistent Exercise
A Positive Mental Attitude
Excellent Nutrition
And Chiropractic
Brain Impulses
Dr. Seth Sharpless at the University of Colorado showed that the weight of a dime on a nerve alters (brain) impulses by 60%.
Vertebral Subluxations

Chiropractic Guidelines

Chiropractic Treatment
Traditional chiropractic care relies on spinal adjustments to correct subluxations (misaligned vertebrae), which may be responsible for pain or problems anywhere along the spine.
Vertebral Subluxations

Chiropractic Treatment
Spinal manipulation, chiropractic’s primary treatment technique, is one of only three treatments whose effectiveness is substantiated by rigorous research.


Results showed that 38 % of patients chose to seek chiropractic care rather than medical care and
…chiropractic was more cost-effective than anesthesiology, neurosurgery, neurology, registered physical therapy, orthopedic reconstructive surgery, physical medicine and rehabilitation, and rheumatology.
The study also showed that most of the chiropractic expenses (89%) were related directly to patient care, while only 45% of the medical costs were related to treatment of the condition with remainder of the costs being for diagnostic procedures such as XRays and MRI’s.

Without these additional costs being included in the study, the costs related to medical care were reported much lower than they actually were, and the savings from chiropractic care were actually much larger.
Chiropractic Treatment Options

Chiropractic Treatment – Canadian Study
In 1985, a landmark study published in the Canadian Family Physician researched the effects of chiropractic adjustments for people with severe and chronic lower back pain.
Approximately 300 subjects had been “totally disabled” by back pain for an average of 7 years, and had gone through the full gamut of standard medical interventions.
The study found that after 2 to 3 weeks of daily chiropractic adjustments, between 79 and 93 % of patients without spinal stenosis (narrowed spinal cord) had good to excellent results, reporting substantially decreased pain and increased mobility.

After chiropractic treatment, over 70 percent of those studied were improved to the point of having no work restrictions.
Moreover, follow-up a year later demonstrated that the changes were long-lasting.
The landmark Canadian study clearly demonstrated the effectiveness of chiropractic adjustments for treating chronic lower back pain, even when standard medical interventions had been exhausted.
Yet, sadly, many physicians are uneducated about the benefits of chiropractic care.
Chiropractic Treatment – Rand Study
In 1992, the widely respected RAND Corporation, headed by Paul Shekelle, M.D., released a study on spinal manipulation for lower back pain.
It marked the first time that representatives of this prestigious group recognized spinal manipulation as an appropriate treatment for lower back pain.
Chiropractic Treatment – AV MED

Chiropractic care
86% of this group were helped.
12 patients diagnosed as needing disc surgery were able to avoid surgery
Savings to AV MED was $250,000
The Benefits of Chiropractic
The studies presented here are good examples of how chiropractic care plays a vital role in restoring patients’ health.
When a chiropractor removes interference to the nervous system by adjusting the spine, communication to and from the brain is restored and the body is better able to heal itself and function WITHOUT pain.
Chiropractic Can Help!
If you or someone you care about is needlessly suffering from back pain, chiropractic may be the answer you’re searching for.
Your First Chiropractic Examination Visit

During your visit, your doctor of chiropractic will perform exams to locate the source of your pain and will ask you questions about your current symptoms and medical history.
Your doctor of chiropractic will also do physical and neurological exams. In the physical exam, your doctor will observe your posture, range of motion, and physical condition, noting movement that causes pain. Your doctor will feel your spine, note its curvature and alignment, and feel for muscle spasm. A check of your shoulder area is also in order. During the neurological exam, your doctor will test your reflexes, muscle strength, other nerve changes, and pain spread.

In some instances, your chiropractor might order tests to help diagnose your condition. An x-ray can show narrowed disc space, fractures, bone spurs, or arthritis. A computerized axial tomography scan (a CT or CAT scan) or a magnetic resonance imaging test (an MRI) can show bulging discs and herniations. If nerve damage is suspected, your doctor may order a special test called ElectroMyoGraphy (an EMG) to measure how quickly your nerves respond.
Doctors of chiropractic are conservative care doctors; their scope of practice does not include the use of drugs or surgery. If your chiropractor diagnoses a condition outside of this conservative scope, such as a neck fracture or an indication of an organic disease, he or she will refer you to the appropriate medical physician or specialist. He or she may also ask for permission to inform your family physician of the care you are receiving to ensure that your chiropractic care and medical care are properly coordinated.
What Causes Back Pain?
The back is a complicated structure of bones, joints, ligaments and muscles. You can sprain ligaments, strain muscles, rupture disks, and irritate joints, all of which can lead to back pain. While sports injuries or accidents can cause back pain, sometimes the simplest of movements—for example, picking up a pencil from the floor— can have painful results. In addition, arthritis, poor posture, obesity, and psychological stress can cause or complicate back pain. Back pain can also directly result from disease of the internal organs, such as kidney stones, kidney infections, blood clots, or bone loss.
Back Pain and the Opioid Epidemic
The opioid epidemic has led many respected health groups to reconsider the value of a conservative approach to low back pain (the most common condition for which opioids are prescribed). Most notably, the American College of Physicians (ACP), the largest medical-specialty society in the world, updated its low back pain treatment guideline in 2017 to support a conservative approach to care.
Published in the Annals of Internal Medicine and based on a review of randomized controlled trials and observational studies, the ACP guideline cites heat therapy, massage, acupuncture and spinal manipulation as noninvasive, nondrug options for low back pain treatment. The guideline further states that only when such treatments provide little or no relief should patients move on to medicines such as ibuprofen or muscle relaxants, which research indicates have limited pain-relief effects. According to ACP, prescription opioids should be a last resort for those suffering from low back pain, as the risk of addiction and overdose may outweigh the benefits.
Tips to Prevent Back Pain
There are several simple strategies that can help to prevent the onset of back pain. Among them:
- Maintain a healthy diet and weight.
- Remain active—under the supervision of your chiropractor.
- Avoid prolonged inactivity or bed rest.
- Warm up or stretch before exercising or physical activities, such as gardening.
- Maintain proper posture.
- Wear comfortable, low-heeled shoes.
- Sleep on a mattress of medium firmness to minimize any curve in your spine.
- When lifting an object, lift with your knees, keep the object close to your body, and do not twist.
- Quit smoking. Smoking impairs blood flow, resulting in oxygen and nutrient deprivation to spinal tissues.
- Work with your chiropractor to ensure that your workstation is ergonomically correct.
Chronic Pain and Depression
Pain serves an important function in our lives. When you suffer an acute injury, pain warns you to stop the activity that is causing the injury and tells you to take care of the affected body part. Chronic pain, on the other hand, persists for weeks, months, or even years. Some people, often older adults, suffer from chronic pain without any definable past injury or signs of body damage. Common chronic pain can be caused by headaches, the low back, and arthritis. Unfortunately, there is scant objective evidence or physical findings to explain such pain.
Until recently, some doctors who could not find a physical cause for a person’s pain simply suggested that it was imaginary—“all in your head.” This is unfortunate because we know that all pain is real and not imagined, except in the most extreme cases of psychosis. Emerging scientific evidence is demonstrating that the nerves in the spinal cord of patients with chronic pain undergo structural changes. Psychological and social issues often amplify the effects of chronic pain. For example, people with chronic pain frequently report a wide range of limitations in family and social roles, such as the inability to perform household or workplace chores, take care of children, or engage in leisure activities. In turn, spouses, children, and co-workers often have to take over these responsibilities. Such changes often lead to depression, agitation, resentment, and anger for the pain patient and to stress and strain in family and other social relationships.
How is depression related to chronic pain?
Depression is the most common emotion associated with chronic pain. It is thought to be three to four times more common in people with chronic pain than in the general population. In addition, 30% to 80% of people with chronic pain will have some type of depression. The combination of chronic pain and depression is often associated with greater disability than either depression or chronic pain alone.
People with chronic pain and depression suffer dramatic changes in their physical, mental, and social well-being—and in their quality of life. Such people often find it difficult to sleep, are easily agitated, cannot perform their normal activities of daily living, cannot concentrate, and are often unable to perform their duties at work. This constellation of disabilities starts a vicious cycle—pain leads to more depression, which leads to more chronic pain. In some cases, the depression occurs before the pain. Until recently, we believed that bed rest after an injury was important for recovery. This has likely resulted in many chronic pain syndromes. Avoiding performing activities that a person believes will cause pain only makes his or her condition worse in many cases.
Depression associated with pain is powerful enough to have a substantial negative impact on the outcome of treatment, including surgery. It is important for your doctor to take into consideration not only biological but also psychological and social issues that pain brings.
How to Cope
The first step in coping with chronic pain is to determine its cause, if possible. Addressing the problem will help the pain subside. In other cases, especially when the pain is chronic, you should try to keep the chronic pain from being the entire focus of your life.
Stay active and do not avoid activities that cause pain simply because they cause pain.The amount and type of activity should be directed by your doctor, so that activities that might actually cause more harm are avoided.
Relaxation training, hypnosis, biofeedback, and guided imagery can help you cope with chronic pain. Cognitive therapy can also help patients recognize destructive patterns of emotion and behavior and help them modify or replace such behaviors and thoughts with more reasonable or supportive ones. Distraction (redirecting your attention away from chronic pain), imagery (going to your “happy place”), and dissociation (detaching yourself from the chronic pain) can be useful.
Involving your family with your recovery may be quite helpful, according to recent scientific evidence.
Feel free to discuss these or other techniques with your doctor of chiropractic. He or she may suggest some simple techniques that may work for you or may refer you to another health care provider for more in-depth training in these techniques.
Signs of Chronic Pain
Some of the common signs and symptoms of chronic pain include:
- Pain beyond six months after an injury
- Allodynia—pain from stimuli which are not normally painful and/or pain that occurs other than in the stimulated area
- Hyperpathia—increased pain from stimuli that are normally painful
- Hypersensation—being overly sensitive to pain
Recognizing Depression
Signs of major clinical depression will occur daily for two weeks or more, and often include many of the following:
- A predominant feeling of sadness; feeling blue, hopeless, or irritable, often with crying spells
- Changes in appetite or weight (loss or gain) and/or sleep (too much or too little)
- Poor concentration or memory
- Feeling restless or fatigued
- Loss of interest or pleasure in usual activities, including sex
- Feeling of worthlessness and/or guilt